Neural Tourniquet: A Breakthrough in Stopping Bleeding
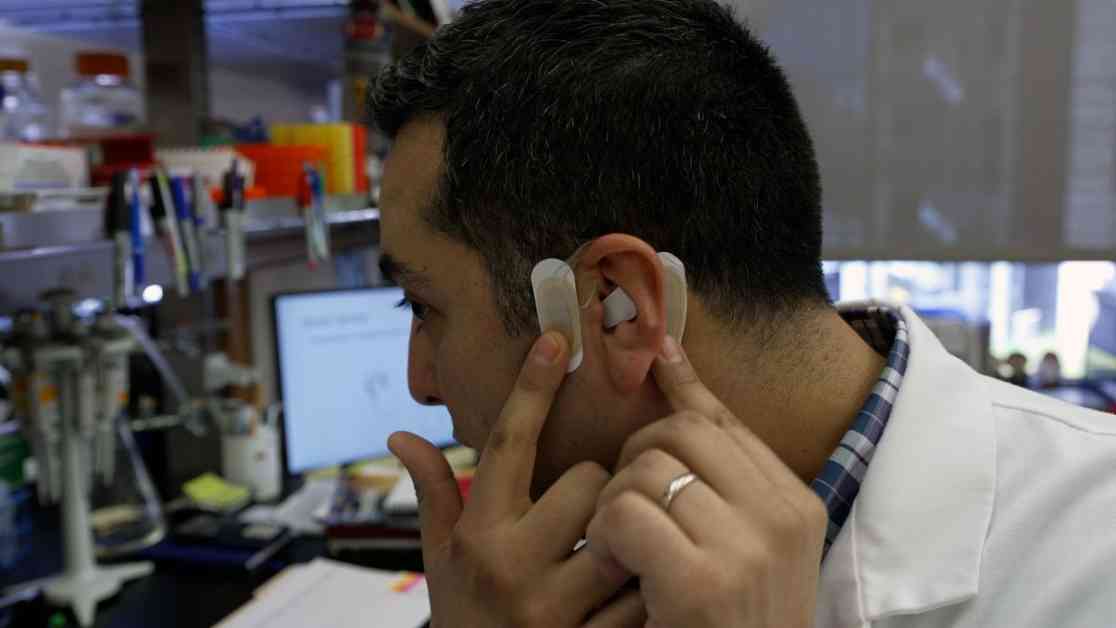
In a groundbreaking development, new research suggests that zapping the vagus nerve could promote blood clotting, potentially revolutionizing surgical procedures. This innovative technique, known as transcutaneous auricular neurostimulation (tAN), was tested in an early trial sponsored by the biomedical company Five Liters. Dr. Jared Huston, a trauma surgeon at the Feinstein Institutes for Medical Research in New York, co-authored the study, heralding the discovery as a potential “neural tourniquet” that could significantly reduce bleeding during surgeries.
The Science Behind the Innovation
The vagus nerve, originating in the brain and extending to various organs, plays a crucial role in controlling the parasympathetic nervous system. Previous experiments on mice and pigs revealed that stimulating the vagus nerve could effectively reduce blood loss. Further investigations by Dr. Huston and his team uncovered the mechanism behind this phenomenon. Through nerve stimulation, immune cells called T cells in the spleen were activated, subsequently triggering platelets to initiate blood clot formation. This groundbreaking research demonstrated the potential of vagus nerve stimulation in enhancing the body’s ability to prevent excessive bleeding.
Implications for Future Medical Practices
While the results of this study are promising, further research is necessary to validate the efficacy of vagus nerve stimulation in humans. Collaborating with Five Liters, Dr. Huston’s team conducted trials on healthy volunteers, observing an increase in blood platelet activation following nerve stimulation. These findings, published on ClinicalTrials.gov, underscore the existence of a neural tourniquet pathway in humans, opening doors for non-invasive interventions to control bleeding.
The Road Ahead: Challenges and Opportunities
Although the potential benefits of vagus nerve stimulation are profound, challenges lie ahead in translating these findings into clinical practice. Experts emphasize the need for comprehensive studies to evaluate the impact of nerve stimulation on bleeding times, volumes, and patient outcomes. Despite the promising nature of this research, the consistency of physiological effects from non-invasive stimulators remains a critical consideration.
As the medical community continues to explore the applications of vagus nerve stimulation, the prospect of integrating this technique into surgical protocols holds significant promise. Dr. Huston envisions a future where pre-emptive measures, such as nerve stimulation, could mitigate the risk of excessive bleeding during surgeries, addressing a crucial unmet need in healthcare.
In conclusion, the discovery of the neural tourniquet represents a significant milestone in medical research, offering a potential solution to enhance surgical safety and patient outcomes. With ongoing advancements in neurostimulation technology, the prospect of leveraging the body’s natural processes to control bleeding holds immense potential for transforming the landscape of surgical interventions.