New research in mice suggests that dysfunctional mitochondria could be linked to the development of Crohn’s disease. Crohn’s disease is a chronic inflammatory disorder that affects the gastrointestinal tract, causing symptoms like lower abdominal pain, bloody diarrhea, and fever. While the exact cause of the condition is unknown, it is believed to be related to immune system dysfunction and possibly genetic factors.
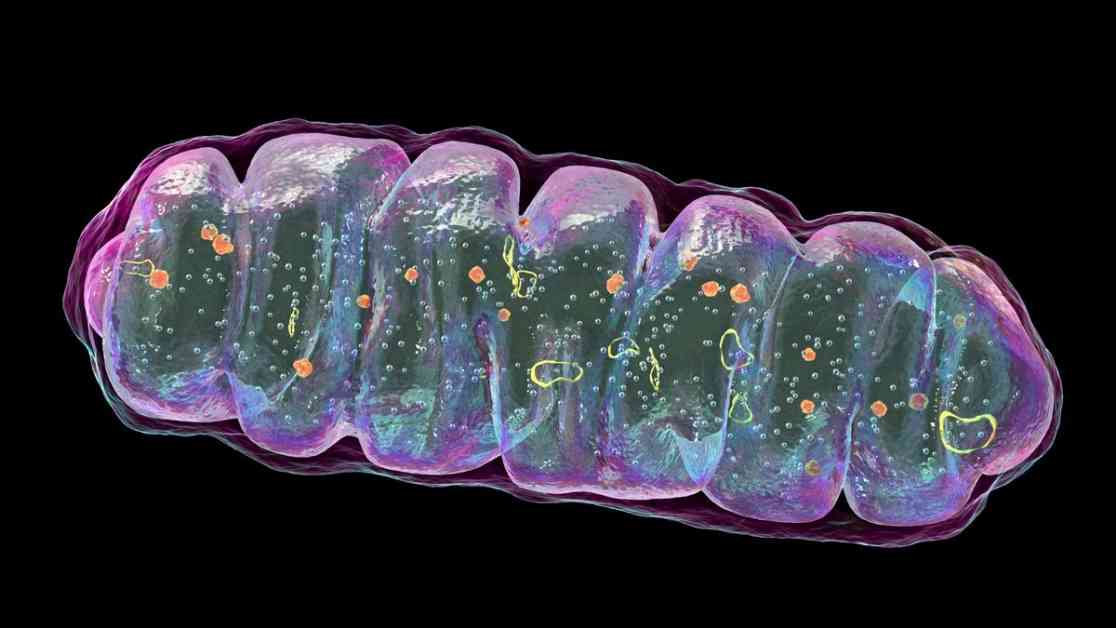
The study, published in the journal Cell Host & Microbe, found that disruptions to mitochondria in the intestine can lead to tissue damage, which in turn alters the composition of the gut microbiome. This alteration in the gut microbiome may be a key factor in triggering the inflammatory process associated with Crohn’s disease.
Researchers bred genetically modified mice that lacked a key mitochondrial protein called HSP60. These mice showed signs of inflammation and tissue injury in their intestines, similar to what is seen in humans with Crohn’s disease. Interestingly, when the mice lacking HSP60 were also bred without gut bacteria, they did not develop any intestinal tissue damage. This suggests that the inflammatory response in Crohn’s may be mediated by intestinal microbes.
Further analysis revealed that a group of gut bacteria called Bacteroides began to dominate the intestines of mice with dysfunctional mitochondria. Bacteroides are normally harmless, but they can become opportunistic pathogens and cause infections when the intestinal wall is compromised. More research is needed to understand why these bacteria thrive after tissue injury and how they contribute to the inflammation seen in Crohn’s disease.
The study authors believe that these findings could lead to the development of targeted treatments for Crohn’s disease in the future. These treatments could potentially act on mitochondria or modify the interactions between mitochondria and the gut microbiome. Understanding the role of mitochondria and gut bacteria in Crohn’s disease could open up new avenues for therapeutic interventions.
While the study was conducted in mice, further research is needed to determine if the same chain reaction occurs in humans. If so, these findings could have significant implications for the treatment of Crohn’s disease. Researchers are hopeful that by unraveling the mechanisms underlying mitochondrial dysfunction and gut microbiome alterations, they can develop more effective therapies for this debilitating condition.